Keratoconus in San Francisco: Your Complete Guide to Diagnosis, Treatment & Living with Confidence
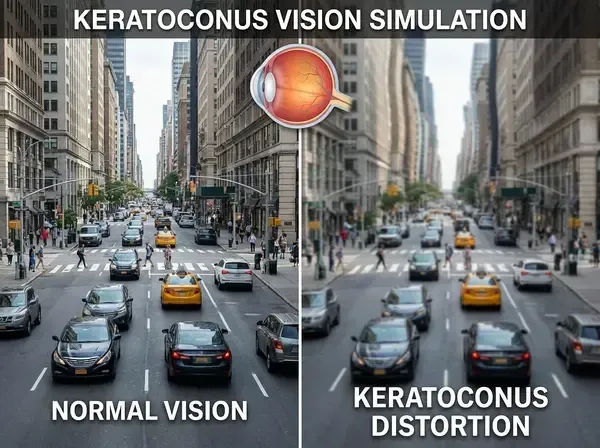
Imagine waking up one morning and noticing that straight lines look curved. Street signs blur no matter how much you squint. Your glasses prescription changes every few months, yet your vision never quite feels "right." You dismiss it as stress, aging, or needing new glasses—until an eye exam reveals the truth: you have keratoconus.
*For the estimated 1 in 2,000 people living with this progressive eye condition, early diagnosis and specialized care make all the difference between preserving clear vision and facing significant visual impairment. In San Francisco's Cow Hollow, Dr. Michelle Blas at Eyes in Disguise combines 30 years of expertise with cutting-edge diagnostic technology to identify ker
atoconus early—often before patients realize anything is wrong—and provides life-changing treatment options that restore visual clarity and confidence.*
Whether you've just been diagnosed, suspect you might have keratoconus, or know you're at risk due to family history, this comprehensive guide covers everything you need to know about living with this condition in 2026.
What is Keratoconus? Understanding the Condition

Keratoconus (pronounced "keh-rah-toh-KOH-nus") is a progressive eye condition where the normally round, dome-shaped cornea—the clear front surface of your eye—gradually thins and bulges outward into a cone-like shape. This irregular shape prevents light from focusing correctly on the retina, causing distorted, blurry vision that standard glasses cannot fully correct.
Breaking down the name:
Kerato= cornea
Conus= cone-shaped
How keratoconus affects your vision:
Under normal circumstances, your cornea maintains a smooth, spherical curvature that bends (refracts) light precisely onto the retina at the back of your eye. When keratoconus develops, the cornea weakens in specific areas, causing:
Irregular astigmatism:The cone-shaped cornea creates multiple focal points instead of one, making vision distorted and wavy
Increasing nearsightedness:As the cornea steepens, myopia progressively worsens
Light sensitivity:The irregular surface scatters light, causing glare and halos around lights
Fluctuating vision:Vision quality can vary hour to hour depending on factors like eye rubbing, allergies, or fatigue
According to the National Keratoconus Foundation, keratoconus typically begins during the teenage years or early 20s and progressively worsens until the mid-30s to early 40s, when it often stabilizes. However, progression rates vary significantly—some patients experience rapid changes over months, while others have slow progression over decades.
The good news?With early detection and appropriate treatment, most people with keratoconus maintain excellent functional vision throughout their lives. Dr. Blas emphasizes that keratoconus is manageable—not a vision-threatening emergency—when caught early and treated properly.
Early Warning Signs: How to Recognize Keratoconus Symptoms
One of the biggest challenges with keratoconus is that early symptoms often mimic more common vision problems. Many patients initially attribute their symptoms to needing new glasses or spending too much time on screens—delaying diagnosis and treatment.
7 Early Warning Signs of Keratoconus
1. Blurry or Distorted Vision That Glasses Don't Fix
If you've recently updated your prescription but straight lines still appear wavy, or if your vision seems "stretched" or shadowed, this could signal irregular astigmatism from keratoconus. Unlike regular astigmatism (which glasses correct easily), keratoconus-related distortion stems from an irregularly shaped cornea that standard lenses cannot fully correct.
2. Rapidly Changing Prescriptions
When glasses prescriptions change significantly every 6-12 months—especially increasing astigmatism or myopia—keratoconus may be the culprit.Modern Optometry reports that progressive prescription changes are often the first red flag that prompts comprehensive corneal evaluation.
3. Increased Sensitivity to Light and Glare
Do car headlights cause excessive glare at night? Do you see halos or starbursts around lights? The irregular corneal surface in keratoconus scatters light, making bright lights uncomfortable and night driving challenging.
4. Trouble Seeing at Night
Beyond glare sensitivity, many keratoconus patients report overall difficulty seeing in low-light conditions. Reading menus in dim restaurants, navigating darkened movie theaters, or driving after sunset becomes progressively harder.
5. Eye Strain, Headaches, and Squinting
When your cornea cannot focus light properly, your eyes work overtime trying to compensate—leading to chronic eye fatigue, frequent headaches (especially after reading or computer work), and constant squinting to improve clarity.
6. Double Vision in One Eye (Monocular Diplopia)
Seeing two overlapping images when viewing with just one eye (the other covered) indicates irregular corneal optics. This differs from binocular double vision (seeing double with both eyes open), which has different causes.
7. One Eye Significantly Worse Than the Other
Keratoconus often affects eyes asymmetrically—one eye may have significant distortion while the other remains relatively normal. If you notice vision quality differs dramatically between eyes, mention this to your optometrist.
Living in San Francisco?Our city's tech-heavy workforce spends countless hours on screens, which can mask early keratoconus symptoms as "digital eye strain." Dr. Blas uses advanced corneal topography during routine exams to distinguish between computer-related fatigue and corneal irregularities—ensuring keratoconus is caught early, when treatment is most effective.
What Causes Keratoconus? Risk Factors & Prevention
While the exact cause of keratoconus remains unclear, research points to a combination of genetic predisposition and environmental triggers. Understanding your risk factors helps with early monitoring and prevention strategies.
Major Risk Factors for Keratoconus
1. Genetics & Family History
About 10-15% of people with keratoconus have a family member with the condition, according to MedlinePlus Genetics. If a parent or sibling has keratoconus, your risk increases significantly—making regular corneal screening essential, even if you have no symptoms.
2. Chronic Eye Rubbing (The #1 Modifiable Risk Factor)

Vigorous, habitual eye rubbing is the most significant behavioral risk factor for keratoconus development and progression. A meta-analysis cited in PMC found that habitual eye rubbers have3 times higher odds of developing keratoconus compared to non-rubbers.
Why eye rubbing is so damaging:
Repeated mechanical trauma weakens corneal collagen structure
Rubbing creates inflammation that further degrades corneal tissue
The combination of pressure and inflammation accelerates cone formation
3. Chronic Allergies & Atopic Conditions
Allergic conjunctivitis, eczema, asthma, and hay fever are strongly associated with keratoconus. The connection? Allergies cause persistent itching, leading to chronic eye rubbing. In San Francisco, where seasonal allergies affect many residents due to eucalyptus pollen, fog exposure, and urban air quality, managing allergies becomes crucial for keratoconus prevention.
4. UV Exposure & Oxidative Stress
Some research suggests chronic UV exposure and oxidative damage contribute to corneal weakening. San Francisco's microclimates mean Cow Hollow, Pacific Heights, and Presidio residents experience varied sun exposure—making quality UV-protective sunglasses essential year-round.
5. Connective Tissue Disorders
Conditions affecting collagen production (like Ehlers-Danlos syndrome, Marfan syndrome, or osteogenesis imperfecta) increase keratoconus risk, as these disorders impact corneal structural integrity.
6. Down Syndrome
Individuals with Down syndrome have significantly elevated keratoconus risk—with some studies showing prevalence rates 10-300 times higher than the general population.
Can You Prevent Keratoconus?
While you cannot prevent genetic predisposition, you can minimize progression risk:
✅STOP rubbing your eyes– Use cold compresses, allergy drops, or antihistamines instead
✅Manage allergies aggressively– Work with Dr. Blas to control itching and inflammation
✅Wear UV-protective sunglasses– 100% UVA/UVB protection, every day, even when foggy
✅Get regular eye exams– Annual corneal topography if you have risk factors
✅Address dry eyes– Dryness triggers rubbing; TearCare® treatment provides relief
How Keratoconus is Diagnosed: Advanced Testing at Eyes in Disguise
Early, accurate diagnosis is the foundation of successful keratoconus management. Dr. Michelle Blas utilizes state-of-the-art diagnostic technology to detect corneal irregularities years before symptoms become severe—often during routine eye exams.
Comprehensive Keratoconus Diagnostic Process
Step 1: Detailed Patient History & Symptom Assessment
Dr. Blas begins by asking targeted questions:
Have you noticed changes in vision quality?
Do you rub your eyes frequently?
Does anyone in your family have keratoconus?
Have your glasses prescriptions changed rapidly?
Do you have allergies, asthma, or eczema?
These questions help identify risk factors and guide testing priorities.
Step 2: Refraction & Visual Acuity Testing
Standard vision testing reveals whether glasses can fully correct your vision. In keratoconus, refraction often shows:
High, irregular astigmatism
Inability to achieve 20/20 vision with best spectacle correction
Significant differences between eyes
Step 3: Slit-Lamp Biomicroscopy
Using a specialized microscope with high magnification, Dr. Blas examines your cornea for keratoconus signs:
Vogt's striae (fine vertical stress lines in the cornea)
Fleischer's ring (iron deposits forming a ring at the cone base)
Corneal thinning or scarring
Prominent corneal nerves
Step 4: Corneal Topography (Corneal Mapping)
This is the gold standard for keratoconus diagnosis. Corneal topography creates a detailed 3D map of your cornea's surface, measuring:
Curvature at thousands of points
Corneal thickness (pachymetry)
Elevation patterns indicating cone formation
Asymmetry between eyes
At Eyes in Disguise, Dr. Blas uses advanced topography systems that detect keratoconus in its earliest stages—often before symptoms appear. Color-coded maps clearly show areas of steepening, allowing Dr. Blas to stage disease severity and track progression over time.
Step 5: Corneal Tomography (Optional for Complex Cases)
For advanced keratoconus or pre-surgical planning, Dr. Blas may recommend Scheimpflug imaging or anterior segment OCT (optical coherence tomography), which provides even more detailed corneal cross-sectional imaging.
Keratoconus Staging: Mild, Moderate, or Advanced?

Keratoconus severity is classified into stages based on corneal steepness (K-reading) and visual impact:
Early/Mild: This stage is characterized by a corneal steepness of less than 48D. The visual distortion is minimal, and glasses may still work effectively. Treatment typically involves monitoring and the use of specialty contact lenses.
Moderate: When corneal steepness reaches between 48-55D, vision distortion becomes more significant, and glasses are no longer effective. Treatment options include scleral lenses and, in some cases, corneal cross-linking.
Advanced: In the advanced stage, corneal steepness exceeds 55D, leading to severe distortion and potential corneal scarring. Treatment options may include scleral lenses, cross-linking, and possibly a corneal transplant.
Why early detection matters:Catching keratoconus in the mild stage opens more treatment options, slows progression, and often prevents the need for surgical intervention.
2026 Keratoconus Treatment Options: From Contact Lenses to Cutting-Edge Therapies
The landscape of keratoconus treatment has transformed dramatically in recent years. Where options were once limited to hard contact lenses or corneal transplants, patients now benefit from multiple effective therapies tailored to disease stage and lifestyle needs.
1. Scleral Contact Lenses: The Gold Standard for Visual Correction

For most keratoconus patients, scleral lenses are life-changing—providing the sharpest vision, all-day comfort, and corneal protection in one elegant solution.
What makes scleral lenses unique:
Unlike traditional contact lenses that rest on the cornea, scleral lenses vault entirely over the irregular corneal surface and rest on the white part of the eye (sclera). The space between the lens and cornea fills with sterile saline, creating a smooth optical surface that corrects even severe irregular astigmatism.
Benefits of scleral lenses for keratoconus:
Unmatched visual clarity:Most patients achieve 20/20 or better vision
All-day comfort:The lens doesn't touch the sensitive cornea
Stability:Large diameter prevents lens displacement or popping out
Corneal protection:The fluid reservoir keeps the cornea hydrated and shields it from environmental irritants
Oxygen permeability:Modern materials allow plenty of oxygen to reach the cornea
Dr. Blas is a specialist in custom scleral lens fitting—a precise art requiring advanced training and experience. Each lens is individually designed based on your unique corneal topography, ensuring optimal fit, comfort, and vision. The fitting process typically involves 2-3 appointments to fine-tune lens parameters.
Cost & insurance:Scleral lenses are a specialty product, with costs typically ranging $800-1,500 per lens plus fitting fees. Many medical insurance plans (not vision insurance) cover scleral lenses for keratoconus as they're medically necessary—Dr. Blas's team assists with insurance authorization.
Learn more in our comprehensive guide:Scleral Contact Lenses in San Francisco
2. Corneal Cross-Linking (CXL): Stopping Progression in Its Tracks
While scleral lenses correct vision, they don't halt keratoconus progression. That's where corneal collagen cross-linking comes in—a revolutionary procedure that strengthens corneal tissue and stops the condition from worsening.
How cross-linking works:
Cross-linking uses riboflavin (vitamin B2) eye drops and controlled ultraviolet (UV) light to create new bonds ("cross-links") between collagen fibers in the cornea. These cross-links reinforce the cornea's structure, preventing further thinning and bulging.
Think of it like adding steel reinforcement to concrete—the cross-links make the cornea stronger and more resistant to progressive deformation.
The FDA-approved procedure (KXL with riboflavin ophthalmic solution):
Riboflavin drops are applied to the cornea
The epithelium (outer corneal layer) may be removed ("epi-off") or left intact ("epi-on")
UV-A light is precisely applied for about 30 minutes
The cornea is monitored during healing
MAJOR 2025 BREAKTHROUGH:In October 2025, the FDA approvedEpioxa™—the first incision-free, epi-on cross-linking treatment. This advancement means:
No removal of the corneal surface
Faster recovery (days vs. weeks)
Less discomfort
Lower infection risk
Who benefits from cross-linking:
Patients with documented keratoconus progression (worsening corneal steepness or vision over 6-12 months)
Teenagers and young adults with early keratoconus
Anyone who wants to prevent future progression
Important note:Cross-linking is a preventative treatment that stops progression—it does NOT reverse existing keratoconus or restore vision. You'll still need contact lenses or glasses for clear vision afterward, but you're preventing the condition from getting worse.
Cross-linking is performed by ophthalmologists, not optometrists.Dr. Blas co-manages keratoconus patients with trusted corneal specialists in San Francisco, coordinating comprehensive care from diagnosis through surgical treatment and post-operative follow-up.
3. Specialty Rigid Gas-Permeable (RGP) Lenses
For patients who aren't candidates for scleral lenses or prefer a smaller lens, traditional rigid gas-permeable contact lenses remain an effective option.
Types of RGP lenses for keratoconus:
Standard RGP lenses:Work well for mild keratoconus
Rose K or other keratoconus-specific designs:Feature special curves designed for cone-shaped corneas
Hybrid lenses:Rigid center for clear optics with soft peripheral skirt for comfort
While RGPs provide excellent vision correction, many patients find sclerals more comfortable for all-day wear.
4. Soft Contact Lenses (Limited Use)
Standard soft lenses rarely provide adequate vision correction for keratoconus due to the irregular corneal shape. However, specialty soft lenses may help mild cases or serve as temporary solutions.
5. Custom Eyeglasses (Mild Cases Only)
In very early keratoconus, high-quality glasses with precise prescriptions may provide adequate vision. However, as the condition progresses, glasses become ineffective due to irregular astigmatism that spectacles cannot correct.
6. Intacs (Corneal Ring Segments)
For moderate keratoconus, tiny plastic ring segments can be surgically inserted into the cornea to flatten the cone and reduce irregular astigmatism. While less common since cross-linking became available, Intacs remain an option when other treatments fail.
7. Corneal Transplant (Last Resort)
When keratoconus is severe, progressed despite cross-linking, or corneal scarring prevents functional vision even with scleral lenses, corneal transplant (keratoplasty) may be necessary. Fortunately, with early detection and modern treatments, only about 10-20% of keratoconus patients eventually need transplants—a dramatic improvement from decades ago.
Types of corneal transplants:
Penetrating keratoplasty (PKP):Full-thickness cornea replacement
Deep anterior lamellar keratoplasty (DALK):Partial-thickness replacement, preserving the innermost corneal layer
Dr. Blas partners with leading corneal transplant surgeons in San Francisco to ensure seamless co-management when surgery becomes necessary.
Living with Keratoconus in San Francisco: Lifestyle Tips & Support
A keratoconus diagnosis can feel overwhelming—but with proper care, most patients live active, fulfilling lives with excellent functional vision. Here's how to thrive with keratoconus in the Bay Area.
5 Essential Lifestyle Strategies
1. Prioritize Allergy Management
San Francisco's unique climate brings seasonal allergens—eucalyptus pollen in spring, grass pollen in summer, and mold spores year-round in foggy neighborhoods like Cow Hollow and the Presidio.
Allergy management tips:
Use daily antihistamine eye drops (prescription-strength like Pataday or Lastacaft)
Take oral antihistamines during peak allergy seasons
Apply cool compresses instead of rubbing itchy eyes
Keep bedroom windows closed during high-pollen days
Use HEPA air purifiers
Dr. Blas can prescribe stronger allergy medications if over-the-counter options aren't sufficient.
2. Break the Eye-Rubbing Habit
Stopping eye rubbing is the single most important thing you can do to slow keratoconus progression. But breaking a lifelong habit isn't easy.
Strategies to stop rubbing:
Identify triggers (allergies, fatigue, stress, dry eyes) and address them
Keep hands busy with stress balls or fidget tools
Apply cold compresses when you feel the urge to rub
Wear sleep masks at night to prevent unconscious rubbing
Use preservative-free artificial tears to relieve irritation
Consider TearCare® dry eye treatment if dryness triggers rubbing
3. Protect Your Eyes from UV Exposure
Even on foggy San Francisco days, UV rays penetrate clouds and cause oxidative damage to weakened corneas.
UV protection essentials:
Wear polarized sunglasses with 100% UVA/UVB protection daily
Choose wraparound styles for maximum coverage
Add UV-blocking coatings to prescription glasses
Wear wide-brimmed hats when hiking in Marin, walking the Presidio, or spending time at Ocean Beach
At Eyes in Disguise, Dr. Blas offers designer sunglasses with prescription lenses and superior UV protection—blending medical necessity with luxury style.
4. Maintain Regular Monitoring
Keratoconus requires consistent follow-up to track progression and adjust treatment as needed.
Recommended exam schedule:
Newly diagnosed:Every 3-6 months for first year
Stable keratoconus:Every 6-12 months
Progressive keratoconus:Every 3 months until stabilized
Post-cross-linking:Follow surgeon's protocol (typically 1 week, 1 month, 3 months, 6 months, then annually)
Scleral lens wearers:Annual lens evaluation and corneal health check
5. Connect with Support Resources
You're not alone—thousands of San Francisco residents live successfully with keratoconus.
Support resources:
National Keratoconus Foundation– Educational resources, patient forums, research updates
Eyes in Disguise patient community– Connect with other keratoconus patients in Dr. Blas's practice
Local support groups – Ask Dr. Blas's team for referrals to Bay Area keratoconus meetups
Why Choose Eyes in Disguise for Keratoconus Care in San Francisco?
Managing keratoconus requires specialized expertise, advanced technology, and a personalized approach—qualities that define Dr. Michelle Blas's practice in Cow Hollow.
What Sets Dr. Blas Apart:
30+ Years of Advanced Optometric Experience
Dr. Blas has dedicated three decades to mastering complex vision correction, including specialty contact lens fitting for irregular corneas. Her extensive experience means she's seen thousands of keratoconus presentations—from subtle early cases to advanced scenarios—and knows exactly how to optimize outcomes.
State-of-the-Art Diagnostic Technology
Eyes in Disguise features the same corneal topography and imaging systems used by leading corneal specialists, ensuring accurate diagnosis and precise treatment planning. Dr. Blas doesn't just identify keratoconus—she quantifies progression, predicts outcomes, and customizes treatment strategies based on objective data.
Expert Scleral Lens Fitting
Scleral lens fitting is an art requiring specialized training and experience. Dr. Blas has fitted hundreds of scleral lenses for keratoconus patients, mastering the nuances that make the difference between "good enough" and "life-changing" vision.
Collaborative Care Model
When cross-linking, Intacs, or transplant surgery becomes necessary, Dr. Blas partners with San Francisco's top corneal surgeons—ensuring seamless co-management from pre-operative planning through post-surgical recovery and long-term follow-up.
Luxury Experience Meets Medical Excellence
Located in the heart of Cow Hollow, Eyes in Disguise combines clinical expertise with a boutique, personalized experience. You're not a number—you're a valued patient receiving individualized attention in an elegant setting.
Same-Day Emergency Care
Keratoconus complications—like contact lens-related issues, corneal abrasions, or sudden vision changes—require prompt attention. Eyes in Disguise offers same-day emergency appointments, ensuring you're never left waiting when urgent problems arise.
Frequently Asked Questions About Keratoconus
1. Is keratoconus hereditary? Should my children be screened?
About 10-15% of keratoconus patients have a family history. If you have keratoconus, your children have elevated risk and should undergo baseline corneal topography screening by their teenage years—even without symptoms. Early detection in children allows intervention before significant progression occurs.
2. Will I go blind from keratoconus?
No—keratoconus rarely causes complete blindness. While it significantly impacts vision quality, modern treatments (especially scleral lenses and cross-linking) allow most patients to maintain excellent functional vision throughout life. Even in severe cases requiring corneal transplant, vision can typically be restored.
3. How long do scleral lenses last for keratoconus?
With proper care, scleral lenses typically last 1-3 years before needing replacement. However, if your keratoconus progresses (especially before cross-linking), you may need lens replacement sooner to match your changing corneal shape. Dr. Blas monitors both lens condition and corneal changes at annual visits.
4. Does insurance cover keratoconus treatment in San Francisco?
Most medical insurance plans (not vision insurance) cover medically necessary keratoconus treatments, including scleral lenses, specialty contact lenses, and corneal cross-linking. Coverage varies by plan—Eyes in Disguise's insurance specialists verify benefits and handle pre-authorizations to maximize your coverage.
5. Can I still drive with keratoconus?
Yes, most keratoconus patients drive safely with proper correction (usually scleral or specialty RGP lenses). However, night driving can be challenging due to glare and halos from lights. Dr. Blas ensures your vision meets legal driving requirements and offers strategies to minimize nighttime visual difficulties.
6. Will keratoconus get worse as I age?
Keratoconus typically progresses most rapidly during the teens and twenties, then stabilizes in the mid-30s to early 40s. However, progression patterns vary—some patients remain stable for decades, while others experience changes later in life. Regular monitoring detects progression early, allowing timely intervention.
7. Can I have LASIK if I have keratoconus?
No—LASIK and PRK (laser vision correction) are contraindicated in keratoconus because they further thin the already-weakened cornea, potentially causing rapid progression or ectasia (corneal bulging). In fact, advanced screening now detects subtle keratoconus patterns before LASIK to prevent this complication.
8. What's the difference between an optometrist and ophthalmologist for keratoconus?
Optometrists like Dr. Blas diagnose keratoconus, prescribe specialty contact lenses (including scleral lenses), manage ongoing care, and co-manage surgical patients. Ophthalmologists perform surgical treatments like cross-linking, Intacs, and corneal transplants. Most keratoconus patients see their optometrist for regular care and only visit an ophthalmologist if surgery becomes necessary.
AUTHOR BIO
Dr. Michelle Blas, OD, has served San Francisco's Cow Hollow, Pacific Heights, Fillmore, and Presidio neighborhoods for over 30 years, specializing in advanced contact lens fitting for complex corneal conditions including keratoconus. As an expert in scleral lens design and fitting, Dr. Blas has helped hundreds of keratoconus patients achieve life-changing visual clarity. At Eyes in Disguise, she combines cutting-edge diagnostic technology with personalized, luxury care—ensuring every patient receives the attention and expertise their vision deserves.
Suspect you might have keratoconus? Schedule a comprehensive eye exam with Dr. Blas at Eyes in Disguise today. Early detection changes everything. Call (415) 474-5321 or book your appointment online.
FAQ SECTION
1. What are the first signs of keratoconus?
The earliest signs of keratoconus include blurry or distorted vision that glasses don't fully correct, rapidly changing prescriptions every 6-12 months, increased sensitivity to light and glare, and difficulty seeing at night. Many patients also experience frequent eye strain, headaches, and notice straight lines appearing wavy or curved. If you notice any of these symptoms, schedule a comprehensive eye exam with corneal topography at Eyes in Disguise in San Francisco.
2. How is keratoconus diagnosed in San Francisco?
Keratoconus is diagnosed using corneal topography—a painless imaging test that creates a detailed 3D map of your cornea's shape. Dr. Michelle Blas uses advanced topography systems at Eyes in Disguise to detect even subtle corneal irregularities indicative of early keratoconus. The exam also includes refraction testing, slit-lamp examination, and detailed patient history to confirm diagnosis and stage severity. Most exams take 30-45 minutes.
3. What is the best treatment for keratoconus in 2026?
The best keratoconus treatment depends on disease stage and progression. For vision correction, scleral contact lenses are the gold standard—providing excellent visual clarity and all-day comfort for most patients. To stop progression, corneal cross-linking (including the new FDA-approved Epioxa™ epi-on procedure) strengthens the cornea and prevents worsening. Dr. Blas at Eyes in Disguise specializes in scleral lens fitting and co-manages cross-linking with San Francisco's top corneal surgeons.
4. Can scleral lenses fix keratoconus vision problems?
Yes—scleral lenses provide excellent vision correction for keratoconus by vaulting over the irregular cornea and creating a smooth optical surface. Most keratoconus patients achieve 20/20 or better vision with properly fitted scleral lenses. Dr. Blas is an expert in custom scleral lens fitting at Eyes in Disguise in Cow Hollow, designing each lens based on your unique corneal topography for optimal vision, comfort, and corneal health.
5. Does insurance cover keratoconus treatment in San Francisco?
Most medical insurance plans (not vision insurance) cover medically necessary keratoconus treatments, including scleral lenses, specialty contact lenses, and corneal cross-linking procedures. Coverage varies by plan and may require pre-authorization. The team at Eyes in Disguise verifies your insurance benefits, handles pre-authorization paperwork, and helps maximize your coverage for keratoconus treatment.
6. Will my keratoconus get worse over time?
Keratoconus typically progresses fastest during the teenage years and twenties, then often stabilizes in the mid-30s to early 40s. However, progression varies significantly between individuals. The most important factor you control is avoiding eye rubbing—habitual rubbers have 3 times higher progression risk. Corneal cross-linking can halt progression entirely. Dr. Blas monitors keratoconus patients every 3-12 months to detect progression early and adjust treatment as needed.
7. Is keratoconus hereditary? Should my children be tested?
About 10-15% of keratoconus patients have a family member with the condition, indicating genetic components. If you have keratoconus, your children have elevated risk and should undergo baseline corneal topography screening by their teenage years—even without symptoms. Dr. Blas recommends early screening for children of keratoconus patients at Eyes in Disguise, as early detection allows intervention before significant vision impairment occurs.
8. Can I still drive safely with keratoconus in California?
Yes, most keratoconus patients drive safely with proper vision correction—usually scleral or specialty rigid gas-permeable contact lenses. California DMV requires minimum 20/40 vision in at least one eye for an unrestricted license. Dr. Blas ensures your vision meets legal requirements and provides strategies to manage night-driving challenges like glare and halos. If vision doesn't meet standards with correction, DMV may require testing or restrictions.